Symptoms of Narcolepsy
This content was developed using the International Classification of Sleep Disorders, third edition, text revision (ICSD-3-TR) and other materials.
Symptoms of Narcolepsy
This content was developed using the International Classification of Sleep Disorders, third edition, text revision (ICSD-3-TR) and other materials.
Overview
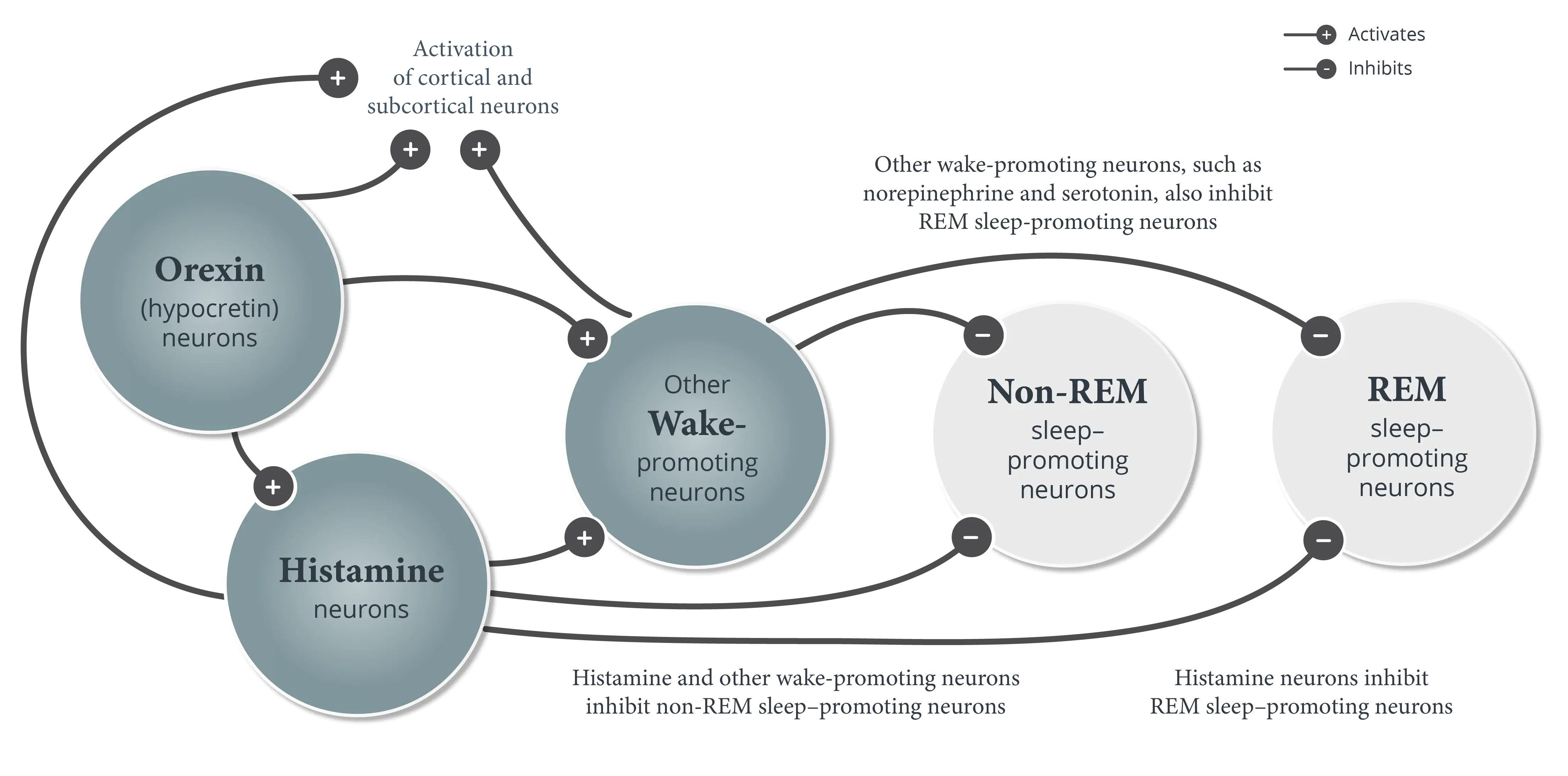
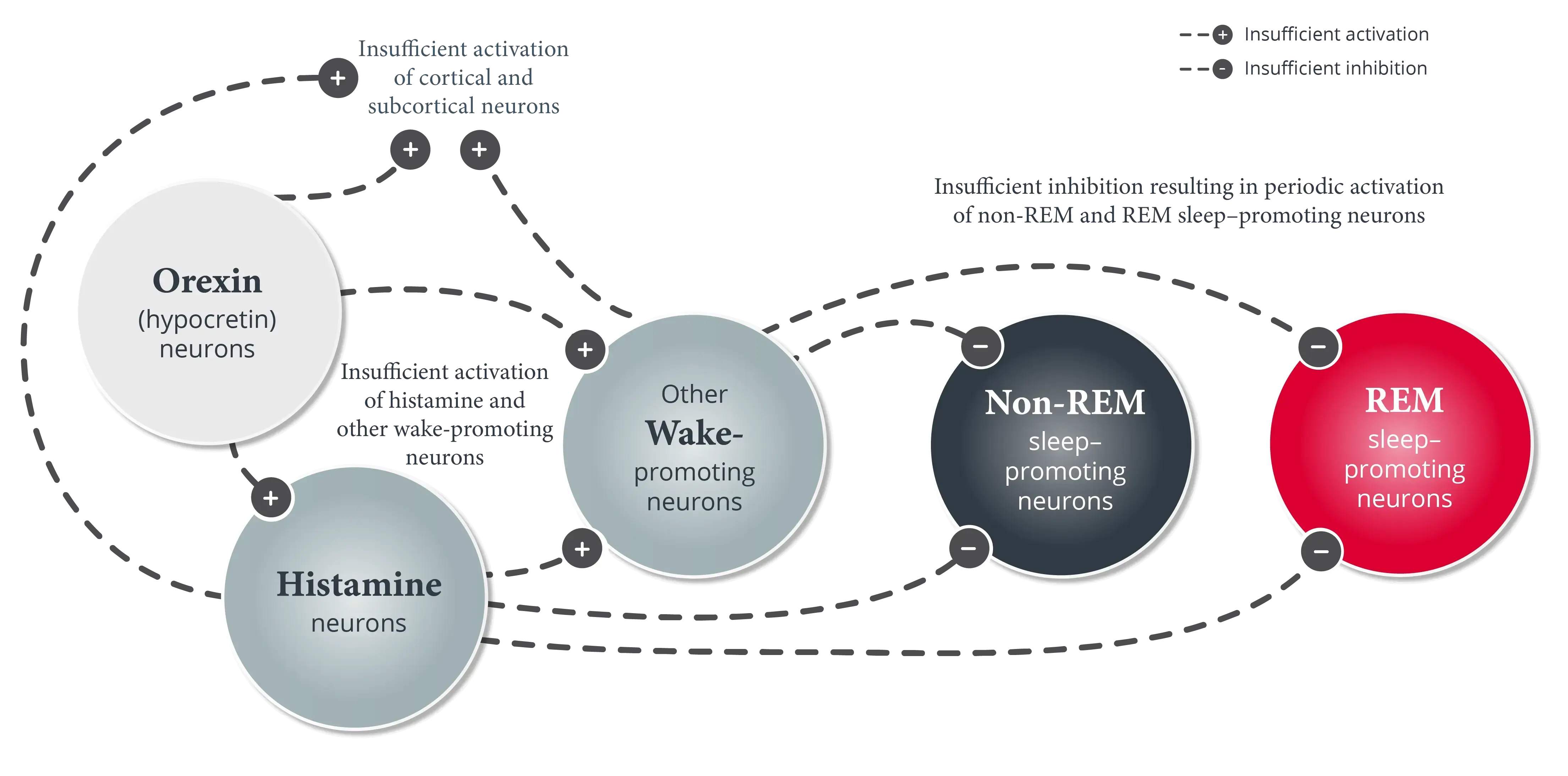
Narcolepsy is a chronic and lifelong neurologic disorder of sleep-wake state instability characterized by excessive daytime sleepiness (EDS) and abnormal manifestations of REM sleep.1-3
Symptoms of Narcolepsy in Adult Patients downloadable presentation
Download this mini presentation for a summary of the symptoms of narcolepsy.
Evaluating narcolepsy in the clinical setting can be difficult.1,4,5 Patients may not always accurately report their symptoms because they may be unaware of the symptoms themselves, including their impact or relationship to sleep.5,6 Although EDS is a core symptom of narcolepsy, continuous assessment of all symptoms is crucial for a comprehensive evaluation.1,5,6
EDS
EDS is the primary symptom of narcolepsy and is often debilitating.1,7 It can cause obvious changes in wakefulness, such as brief lapses into sleep.1,2,6 Most patients awaken feeling refreshed after a sleep episode but begin to feel sleepy again shortly thereafter.1
EDS can also express itself in less obvious ways.2,7 For example, even when seemingly awake, patients with narcolepsy may not feel completely alert.1,2,8 They often experience issues with attention or memory, poor decision-making, and trouble following a conversation.2,7 These issues can have a serious impact on functioning in educational, social, and occupational settings.1
Cataplexy
Cataplexy rarely presents in a clinical setting, and it can range from obvious to subtle manifestations.1,2,9 Patients experiencing complete cataplexy may collapse to the ground and briefly remain there.1,2 However, more commonly, cataplexy is partial.4,10 It often occurs in the head and neck, manifesting as head drops, but may occur in other areas, such as knee buckling or arm/hand weakness—patients may describe themselves as clumsy or report dropping things.1,2,11 Facial hypotonia is a reliable marker of cataplexy and manifests as abrupt interruption of the smile or facial expression, mouth opening, and sagging of the jaw or eye muscles.2,11,12
Disrupted nighttime sleep
Many patients with narcolepsy have disrupted nighttime sleep, reporting frequent awakenings and poor-quality sleep, although they rarely report problems with sleep onset.1,13 Many may report inability to sleep through the night as a significant lifestyle limitation and more of a problem than other symptoms.1,14 Disrupted nighttime sleep can sometimes be misinterpreted and misreported by patients as insomnia due to their similarities.13
Hypnagogic/hypnopompic hallucinations
About one-third of all patients with narcolepsy have vivid, dreamlike experiences during the transition from wake to sleep (hypnagogic hallucinations) or during the transition from sleep to wake (hypnopompic hallucinations).1,6 Patients may see lifelike phenomena that can be realistic and frightening, including dark shadows, or threatening figures, animals, or people.6,10,15
Automatic behavior
Patients may also experience automatic behaviors during microsleep episodes, in which they perform everyday activities without any memory of doing so. This happens because patients may not be fully awake and alert, affecting memory formation.2 For example, patients may place unusual objects in the refrigerator; this can indicate these automatic behaviors are happening even if they have no recollection of the activity.2,6
Even when seemingly awake, most patients with narcolepsy have impaired sustained attention, sometimes in combination with automatic behavior such as writing gibberish or interrupting a conversation with a completely different topic. Sleepiness and impaired sustained attention often have serious impacts on the ability of the patient to function properly in educational, social, and occupational situations.1
Sleep paralysis
Sleep paralysis may occur together with hypnagogic or hypnopompic hallucinations; it usually occurs at the point of waking but may also occur at sleep onset.1,6 During these episodes, patients may feel like they are being suffocated or weighed down, and they may become frightened or have anxiety associated with fear that they are dying.6,11,15
Get more insights that can help in evaluating the symptoms of narcolepsy.
References
- American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd ed, text revision. American Academy of Sleep Medicine; 2023.
- Thorpy M, Morse AM. Reducing the clinical and socioeconomic burden of narcolepsy by earlier diagnosis and effective treatment. Sleep Med Clin. 2017;12(1):61-71.
- Thorpy MJ, Bogan RK. Update on the pharmacologic management of narcolepsy: mechanisms of action and clinical implications. Sleep Med. 2020;68:97-109.
- Overeem S. The clinical features of cataplexy. In: Baumann CR, Bassetti CL, Scammell TE, eds. Narcolepsy: Pathophysiology, Diagnosis, and Treatment. Springer-Verlag New York; 2011:283-290.
- Thorpy MJ, Dauvilliers Y. Clinical and practical considerations in the pharmacologic management of narcolepsy. Sleep Med. 2015;16(1):9-18.
- Overeem S, Reading P, Bassetti CL. Narcolepsy. Sleep Med Clin. 2012;7(2):263-281.
- Ahmed IM, Thorpy MJ. Clinical evaluation of the patient with excessive sleepiness. In: Thorpy MJ, Billiard M, eds. Sleepiness: Causes, Consequences and Treatment. Cambridge University Press; 2011:36-47.
- Nishino S. Clinical and neurobiological aspects of narcolepsy. Sleep Med. 2007;8(4):373-399.
- Dauvilliers Y, Siegel JM, Lopez R, Torontali ZA, Peever JH. Cataplexy—clinical aspects, pathophysiology and management strategy. Nat Rev Neurol. 2014;10(7):386-395.
- Ahmed I, Thorpy M. Clinical features, diagnosis and treatment of narcolepsy. Clin Chest Med. 2010;31(2):371-381.
- Pelayo R, Lopes MC. Narcolepsy. In: Lee-Chiong TL, ed. Sleep: A Comprehensive Handbook. John Wiley & Sons; 2006:145-149.
- Pizza F, Antelmi E, Vandi S, et al. The distinguishing motor features of cataplexy: a study from video-recorded attacks. Sleep. 2018;41(5). doi:10.1093/sleep/zsy026
- Roth T, Dauvilliers Y, Mignot E, et al. Disrupted nighttime sleep in narcolepsy. J Clin Sleep Med. 2013;9(9):955-965.
- Maski K, Steinhart E, Williams D, et al. Listening to the patient voice in narcolepsy: diagnostic delay, disease burden, and treatment efficacy. J Clin Sleep Med. 2017;13(3):419-425.
- Dauvilliers Y, Lopez R. Parasomnias in narcolepsy with cataplexy. In: Baumann CR, Bassetti CL, Scammell TE, eds. Narcolepsy: Pathophysiology, Diagnosis, and Treatment. Springer-Verlag New York; 2011:291-299.