Pathophysiology of Narcolepsy
This content was developed using literature published in peer-reviewed journals and other materials from experts in sleep medicine.
Pathophysiology of Narcolepsy
This content was developed using literature published in peer-reviewed journals and other materials from experts in sleep medicine.
Overview
Narcolepsy type 1 is caused by deficiencies in orexin (hypocretin) signaling, most likely due to a selective loss of hypothalamic orexin (hypocretin)-producing neurons due to an autoimmune process. The cause of narcolepsy type 2 is not fully known; a small portion of patients with a diagnosis of narcolepsy type 2 also have low (≤110 pg/mL) or intermediate (>110 pg/mL but ≤200 pg/mL) levels of orexin (hypocretin) in the CSF.1
The pathophysiology of narcolepsy
Learn more about the neuronal processes involved in the sleep-wake state instability resulting from orexin (hypocretin) loss in narcolepsy.1,2
Pathophysiology downloadable presentation
Download this mini presentation for a summary of the pathophysiology of narcolepsy.
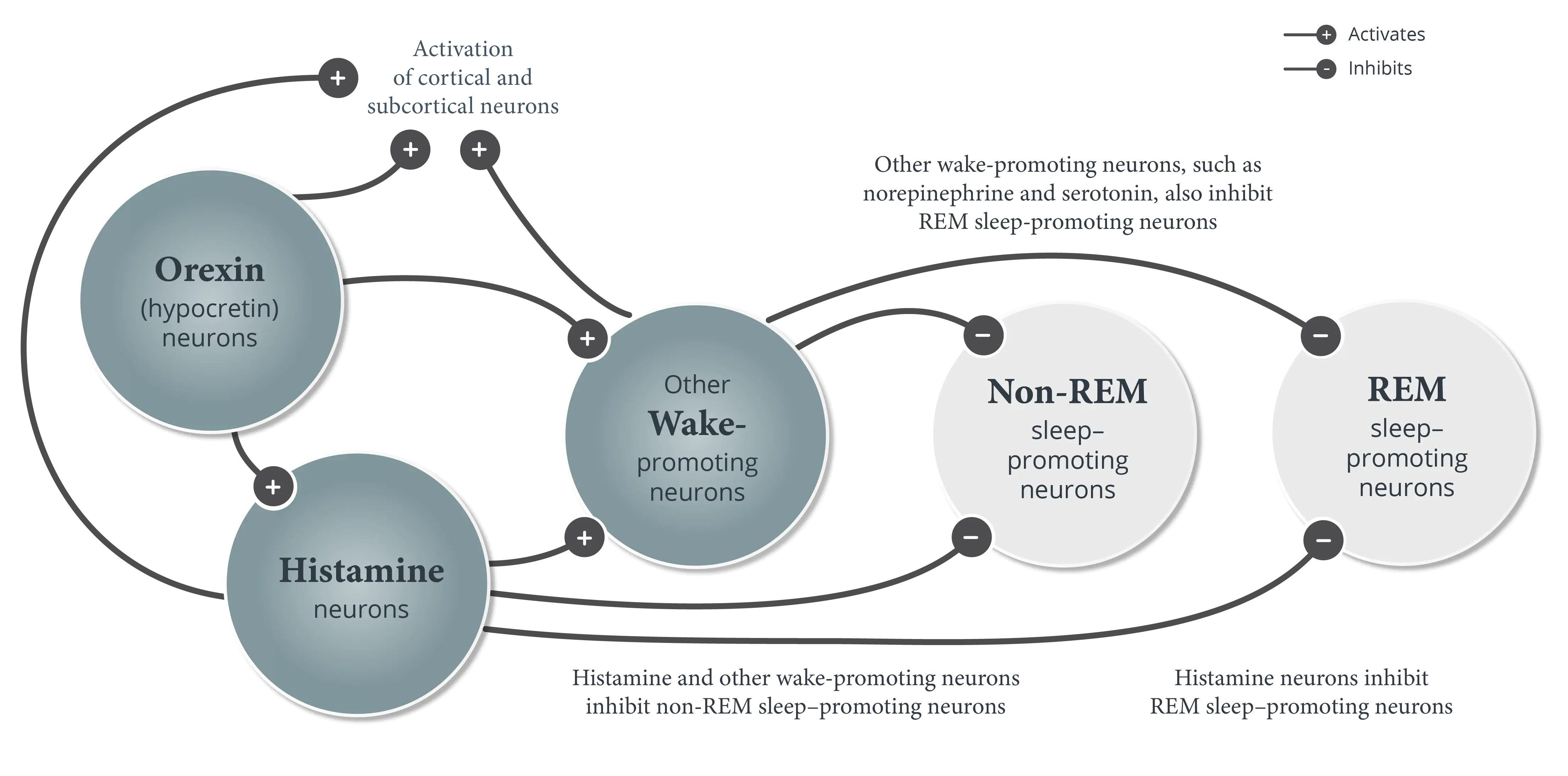
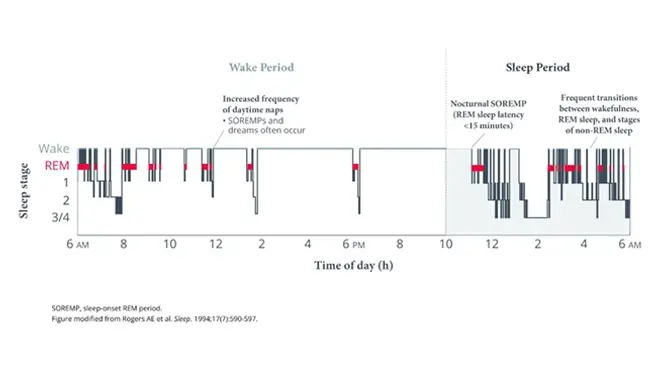
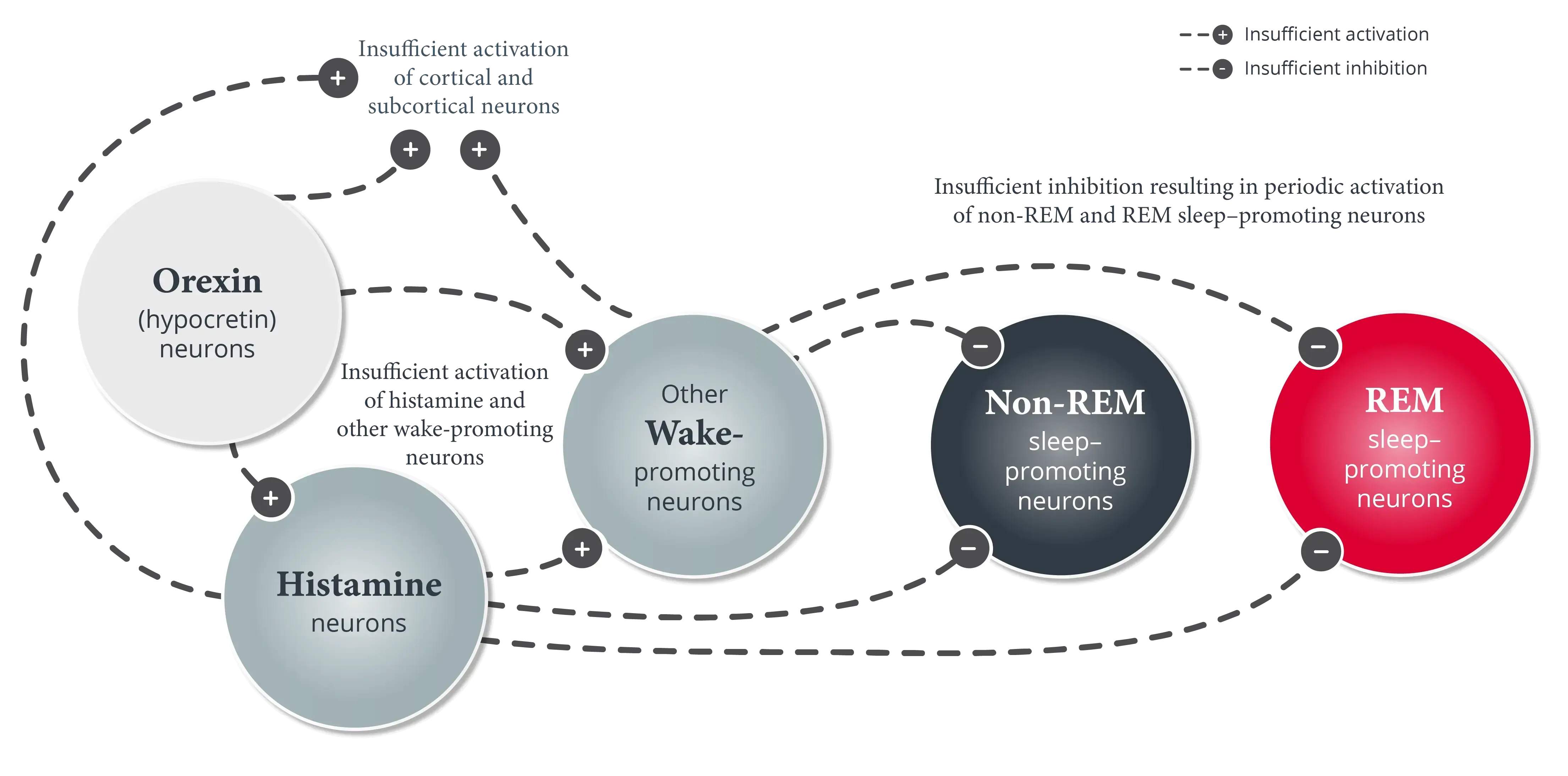
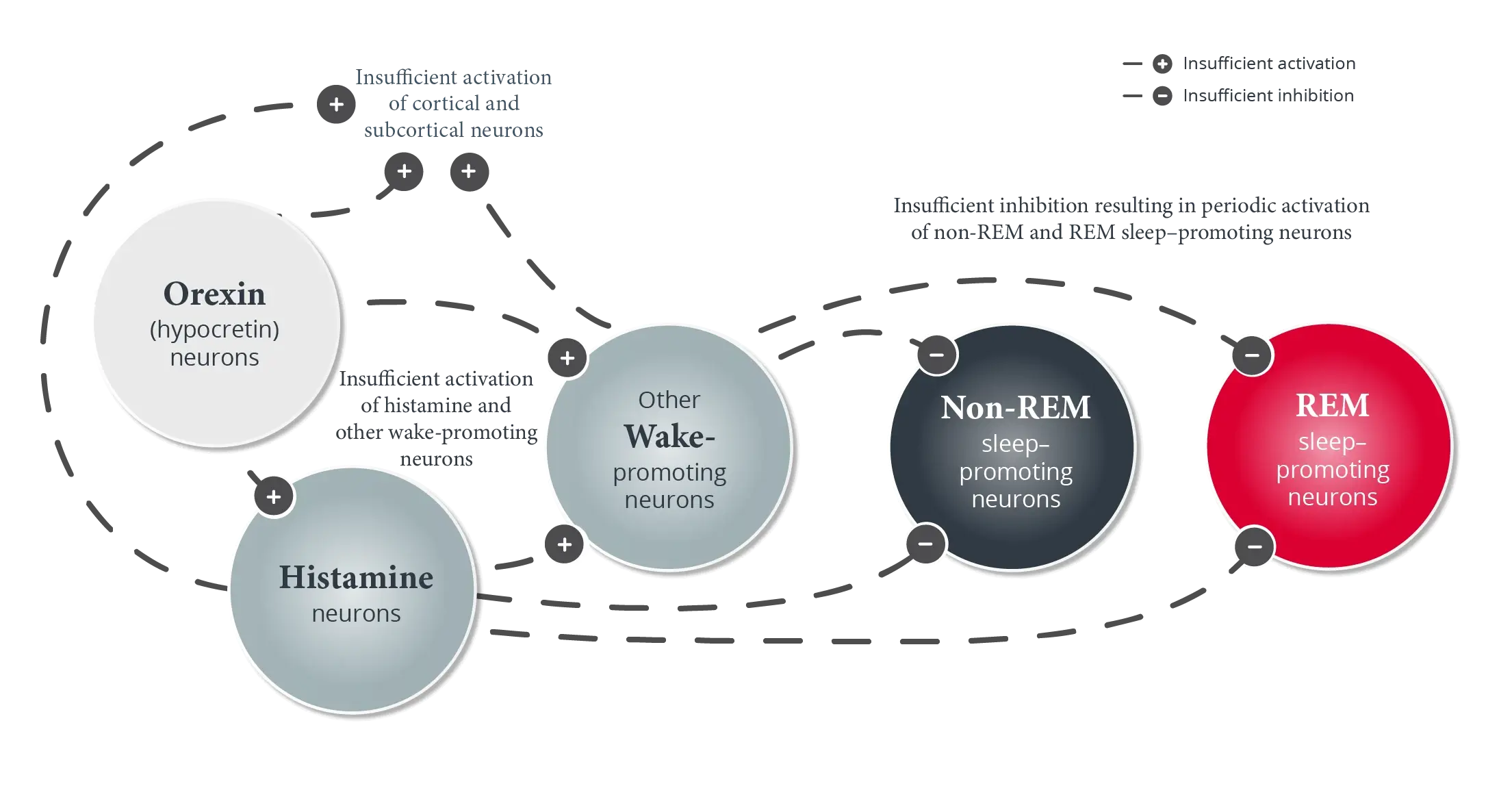
Patients with narcolepsy experience frequent and unpredictable transitions between wakefulness, stages of non-REM sleep, and REM sleep.3-5 In the majority of patients with narcolepsy, this sleep-wake state instability is caused by a loss of orexin (hypocretin) neurons.1,3,4


During the day, lack of orexin (hypocretin) in narcolepsy leads to:
- Insufficient activation of histamine neurons and wake-promoting neurons outside the hypothalamus2,4
- Insufficient inhibition and intermittent activation of non-REM sleep–promoting neurons4,6
- Insufficient inhibition and intermittent activation of REM sleep–promoting neurons4,7,8
This causes sleep-wake state instability, which manifests as frequent and unpredictable transitions between sleep-wake states and unstable boundaries between sleep-wake states, thereby allowing elements of one state to intrude into another.3,5,9
Based on the strong connection to specific human leukocyte antigen (HLA) genetic subtypes, it is thought that there may be a connection between autoimmunity and narcolepsy.1
Review additional symptom manifestations of sleep-wake state instability.
References
- American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd ed, text revision. American Academy of Sleep Medicine; 2023.
- Scammell TE. Narcolepsy. N Engl J Med. 2015;373(27):2654-2662.
- van der Heide A, Lammers GJ. Narcolepsy. In: Thorpy MJ, Billiard M, eds. Sleepiness: Causes, Consequences and Treatment. Cambridge University Press; 2011:111-125.
- Saper CB, Fuller PM, Pedersen NP, Lu J, Scammell TE. Sleep state switching. Neuron. 2010;68(6):1023-1042.
- Ahmed I, Thorpy M. Clinical features, diagnosis and treatment of narcolepsy. Clin Chest Med. 2010;31(2):371-381.
- Mochizuki T, Crocker A, McCormack S, Yanagisawa M, Sakurai T, Scammell TE. Behavioral state instability in orexin knock-out mice. J Neurosci. 2004;24(28):6291-6300.
- Pillen S, Pizza F, Dhondt K, Scammell TE, Overeem S. Cataplexy and its mimics: clinical recognition and management. Curr Treat Options Neurol. 2017;19(6):23.
- Bassetti C, Aldrich MS. Narcolepsy, idiopathic hypersomnia, and periodic hypersomnias. In: Culebras A, ed. Sleep Disorders and Neurological Disease. Marcel Dekker, Inc; 2000:323-354.
- Broughton R, Valley V, Aguirre M, Roberts J, Suwalski W, Dunham W. Excessive daytime sleepiness and the pathophysiology of narcolepsy-cataplexy: a laboratory perspective. Sleep. 1986;9(1 pt 2):205-215.