Subtypes of Narcolepsy
This content was developed using the International Classification of Sleep Disorders, third edition, text revision (ICSD-3-TR), with additional support from published literature.
Subtypes of Narcolepsy
This content was developed using the International Classification of Sleep Disorders, third edition, text revision (ICSD-3-TR), with additional support from published literature.
Overview
Narcolepsy is classified into two subtypes—type 1 and type 2—both of which share the primary symptom of excessive daytime sleepiness (EDS).1
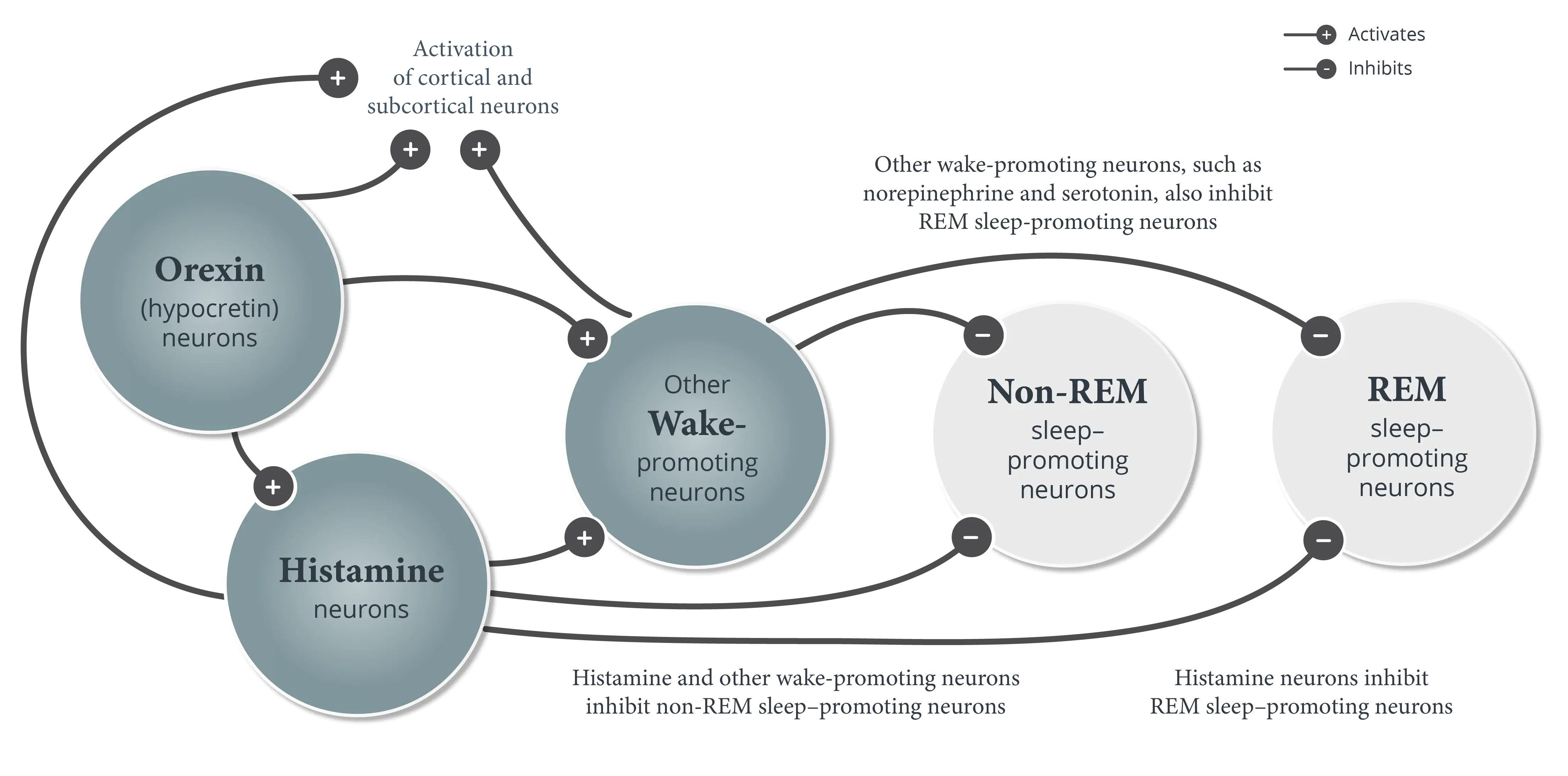
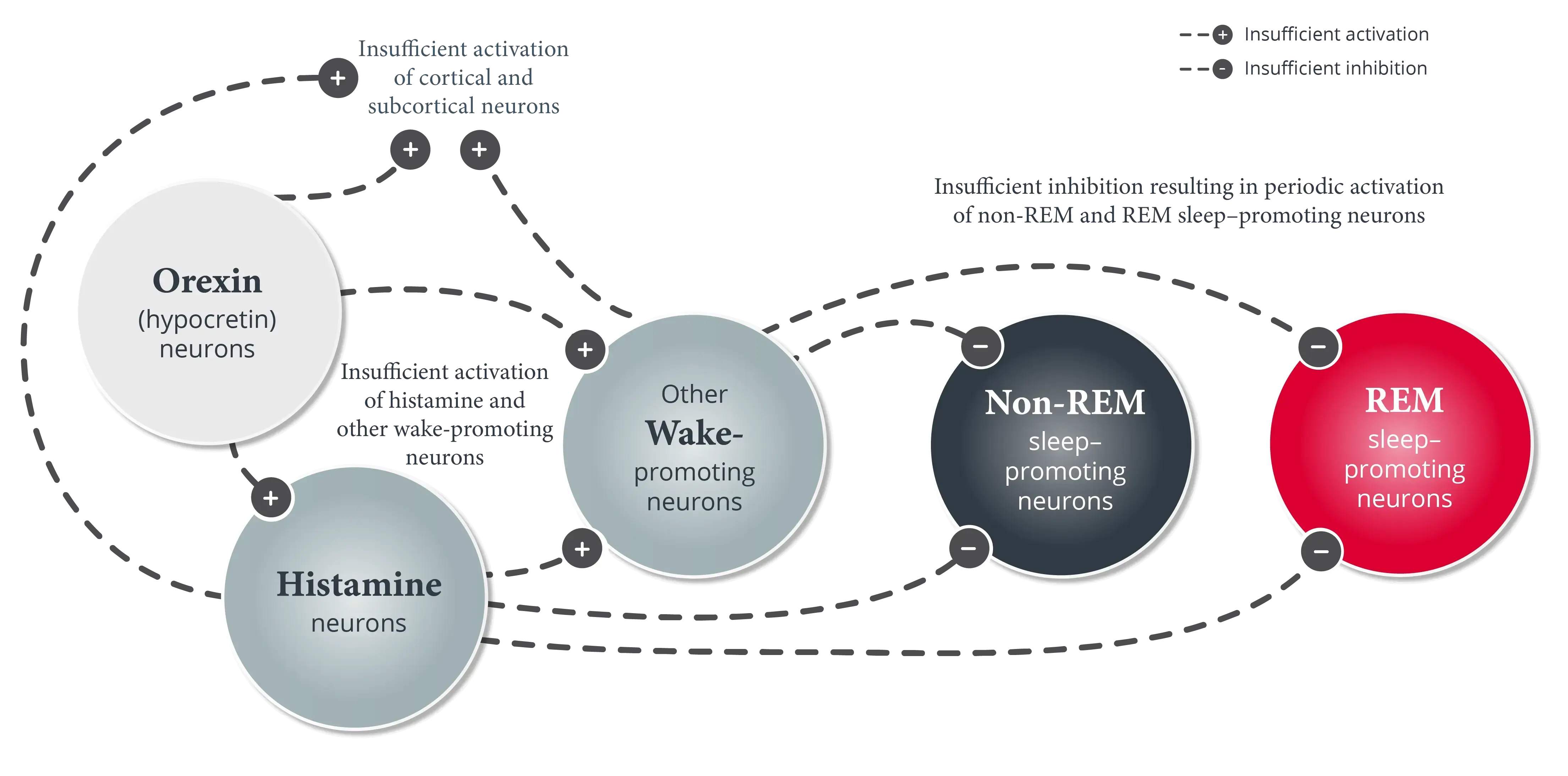
Narcolepsy is diagnosed as either narcolepsy type 1 or narcolepsy type 2. Both share the same primary symptom, excessive daytime sleepiness (EDS), but orexin (hypocretin) deficiency is a fundamental marker of narcolepsy type 1.1
Narcolepsy type 1 (narcolepsy with cataplexy) is primarily characterized by EDS and signs of REM sleep dissociation, the most specific of which is cataplexy.1
Narcolepsy type 1 makes up two-thirds of narcolepsy cases in the United States.2,3 Patients often experience other symptoms of REM sleep dysregulation, including sleep paralysis and hypnagogic or hypnopompic hallucinations (vivid, dreamlike experiences occurring at sleep-wake transitions), neither of which is specific to the disorder, and may also experience disruptions in nighttime sleep.1
The presence of low cerebrospinal fluid (CSF) hypocretin-1 levels ≤110 pg/mL is a defining biomarker for narcolepsy type 1 and can be used as one of the criteria to confirm the diagnosis, but testing of CSF-hypocretin 1 levels is not required. The diagnosis can be made based on the presence of EDS and cataplexy in addition to objective findings on polysomnography (PSG)/a Multiple Sleep Latency Test (MSLT).1
Narcolepsy type 2 (narcolepsy without cataplexy) is characterized by EDS and signs of REM sleep dissociation on PSG/an MSLT (but without cataplexy).1
Although typical cataplexy is absent, some atypical sensations of weakness triggered by unusual emotions like stress and anger may be reported. Patients with narcolepsy type 2 may also experience sleep paralysis, hypnagogic or hypnopompic hallucinations, and nighttime sleep disruption, with the nighttime sleep disruption occurring to a lesser extent than in patients with narcolepsy type 1.1
Diagnosis of narcolepsy type 2 is primarily based on the presence of EDS in the absence of cataplexy, along with signs of REM sleep disruption on PSG/an MSLT and CSF hypocretin-1 levels of >110 pg/mL.1
Review additional diagnostic criteria and clinical resources for tools that can help in evaluating patients for narcolepsy.
References
- American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd ed, text revision. American Academy of Sleep Medicine; 2023.
- Thorpy MJ. Recently approved and upcoming treatments for narcolepsy. CNS Drugs. 2020;34(1):9-27.
- Ruoff C, Rye D. The ICSD-3 and DSM-5 guidelines for diagnosing narcolepsy: clinical relevance and practicality. Curr Med Res Opin. 2016;32(10):1611-1622.