Narcolepsy Diagnostic Criteria
This content was developed from the International Classification of Sleep Disorders, third edition, text revision (ICSD-3-TR).
Narcolepsy Diagnostic Criteria
This content was developed from the International Classification of Sleep Disorders, third edition, text revision (ICSD-3-TR).
Overview
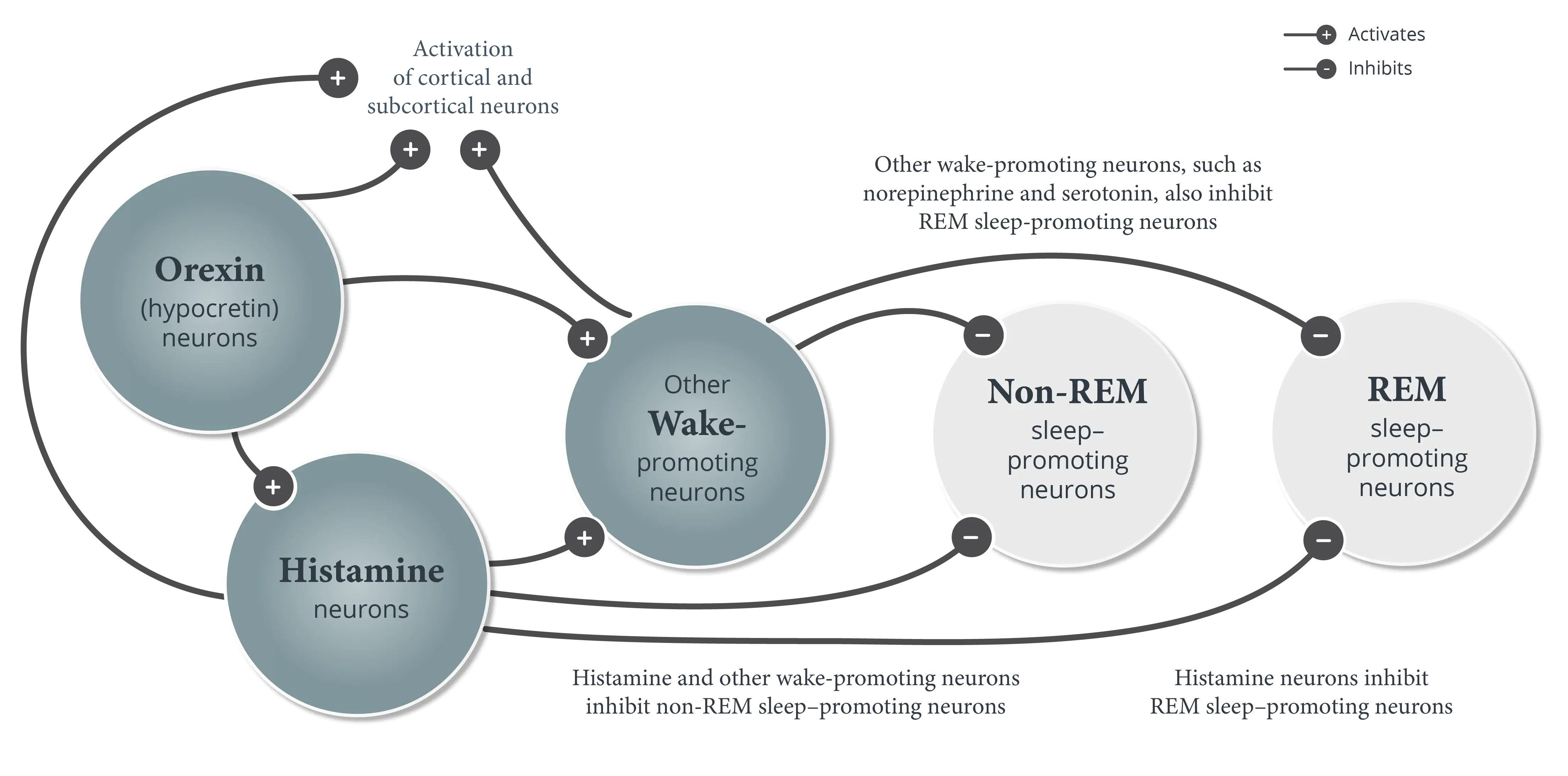
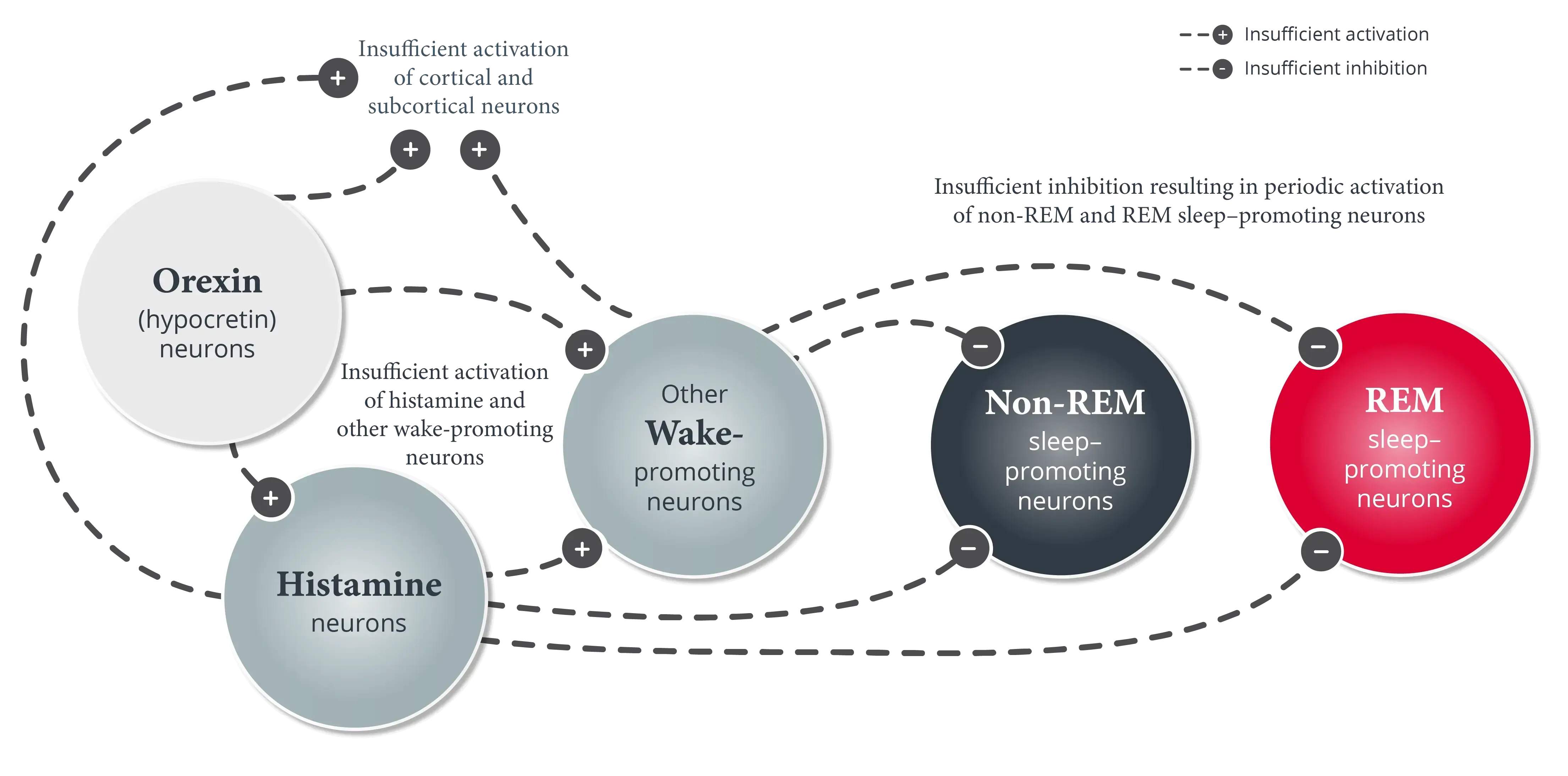
Narcolepsy diagnosis is divided into narcolepsy type 1 and narcolepsy type 2, a distinction based on the presence of cataplexy and/or orexin (hypocretin) deficiency as a fundamental marker of narcolepsy type 1.
Both subtypes of narcolepsy require the presence of excessive daytime sleepiness (EDS), the cardinal symptom of narcolepsy.
Narcolepsy type 1 (narcolepsy with cataplexy)
Criteria A-C must be met:
- The patient has daily periods of irrepressible need to sleep or daytime lapses into drowsiness or sleep
- The presence of least one of the following:
- Cataplexy (as defined under Essential Features in the full ICSD-3-TR diagnostic criteria for narcolepsy type 1)* and either:
- Mean sleep latency of ≤8 minutes and ≥2 sleep-onset REM periods (SOREMPs) on a Multiple Sleep Latency Test (MSLT) performed in accordance with current recommended protocols†
- A SOREMP (within 15 minutes of sleep onset) on nocturnal polysomnogram (PSG)
- Cerebrospinal fluid (CSF) hypocretin-1 concentration, measured by radioimmunoassay, is either ≤110 pg/mL (using a Stanford reference sample) or less than one-third of mean values obtained in normal subjects with the same standardized assay‡
- Cataplexy (as defined under Essential Features in the full ICSD-3-TR diagnostic criteria for narcolepsy type 1)* and either:
- The symptoms and signs are not better explained by chronic insufficient sleep, a circadian rhythm sleep-wake disorder or other current sleep disorder, mental disorder, or medication/substance use or withdrawal
Narcolepsy type 2 (narcolepsy without cataplexy)
Criteria A-E must be met:
- The patient has daily periods of irrepressible need to sleep or daytime lapses into drowsiness or sleep occurring for ≥3 months
- A mean sleep latency of ≤8 minutes and ≥2 SOREMPs on an MSLT performed in accordance with current recommended protocols.† A SOREMP (within 15 minutes of sleep onset) on the preceding nocturnal PSG may replace 1 of the SOREMPs on the MSLT§,¶
- Cataplexy is absent#
- If CSF hypocretin-1 concentration is measured by radioimmunoassay, it is either >110 pg/mL (when using a Stanford reference sample) or more than one-third of mean values obtained in normal subjects with the same standardized assay**
- The symptoms and signs cannot be better explained by chronic insufficient sleep, a circadian rhythm sleep-wake disorder or other current sleep disorder, mental disorder, or medication/substance use or withdrawal
- Typical cataplexy is most strongly associated with narcolepsy type 1. Although some patients with narcolepsy type 1/hypocretin deficiency may present with atypical cataplexy features, presentations that include only atypical cataplexy should raise a higher index of doubt regarding a diagnosis of narcolepsy type 1. Clinical judgment is required. Further guidance regarding distinguishing typical from atypical cataplexy is included in the “Essential Features” section of the diagnostic criteria for narcolepsy type 1 in the full ICSD-3-TR.
- See Krahn LE, Arand DL, Avidan AY, et al. Recommended protocols for the Multiple Sleep Latency Test and Maintenance of Wakefulness Test in adults: guidance from the American Academy of Sleep Medicine. J Clin Sleep Med. 2021;17(12):2489-2498. Sleep logs are required, accompanied by actigraphy, whenever possible, prior to in-laboratory sleep testing to evaluate for insufficient sleep and circadian rhythm disturbances.
- If hypocretin deficiency is verified, the diagnosis of narcolepsy type 1 should be made regardless of other comorbidities that could potentially be related to clinical symptoms, given the definitive nature of this finding.
- The diagnostic value of a SOREMP on nocturnal PSG in the absence of MSLT SOREMPs is not established for narcolepsy type 2. However, it may help guide clinical decision-making, such as the need to pursue repeat or alternative testing.
- Because the circadian clock strongly gates the propensity of REM sleep, narcolepsy type 2 should not be diagnosed in a shift worker without prior re-entrainment to a normal schedule.
- If cataplexy develops later, the disorder should be reclassified as narcolepsy type 1.
- If the CSF hypocretin-1 concentration is tested at a later stage and found to be either ≤110 pg/mL (when using a Stanford reference sample) or less than one-third of mean values obtained in normal subjects with the same standardized assay, the disorder should be reclassified as narcolepsy type 1.
Refer to the full ICSD-3-TR for additional context on diagnostic criteria.
Diagnostic criteria from ICSD-3-TR. Copyright American Academy of Sleep Medicine. Reproduced with permission.
You can also reference the Diagnostic and Statistical Manual of Mental Disorders, 5th edition, text revision (DSM-5-TR) for narcolepsy diagnostic criteria.
In addition to EDS and cataplexy, patients with narcolepsy may report several other symptoms, none of which are specific to the disorder.
References
American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd ed, text revision. American Academy of Sleep Medicine; 2023.