Narcolepsy in Pediatric Patients
This content was developed using the International Classification of Sleep Disorders, third edition, text revision (ICSD-3-TR) and other materials.
Narcolepsy in Pediatric Patients
This content was developed using the International Classification of Sleep Disorders, third edition, text revision (ICSD-3-TR) and other materials.
Overview
Onset of narcolepsy typically begins after age 5, usually between the ages of 7 to 25.1
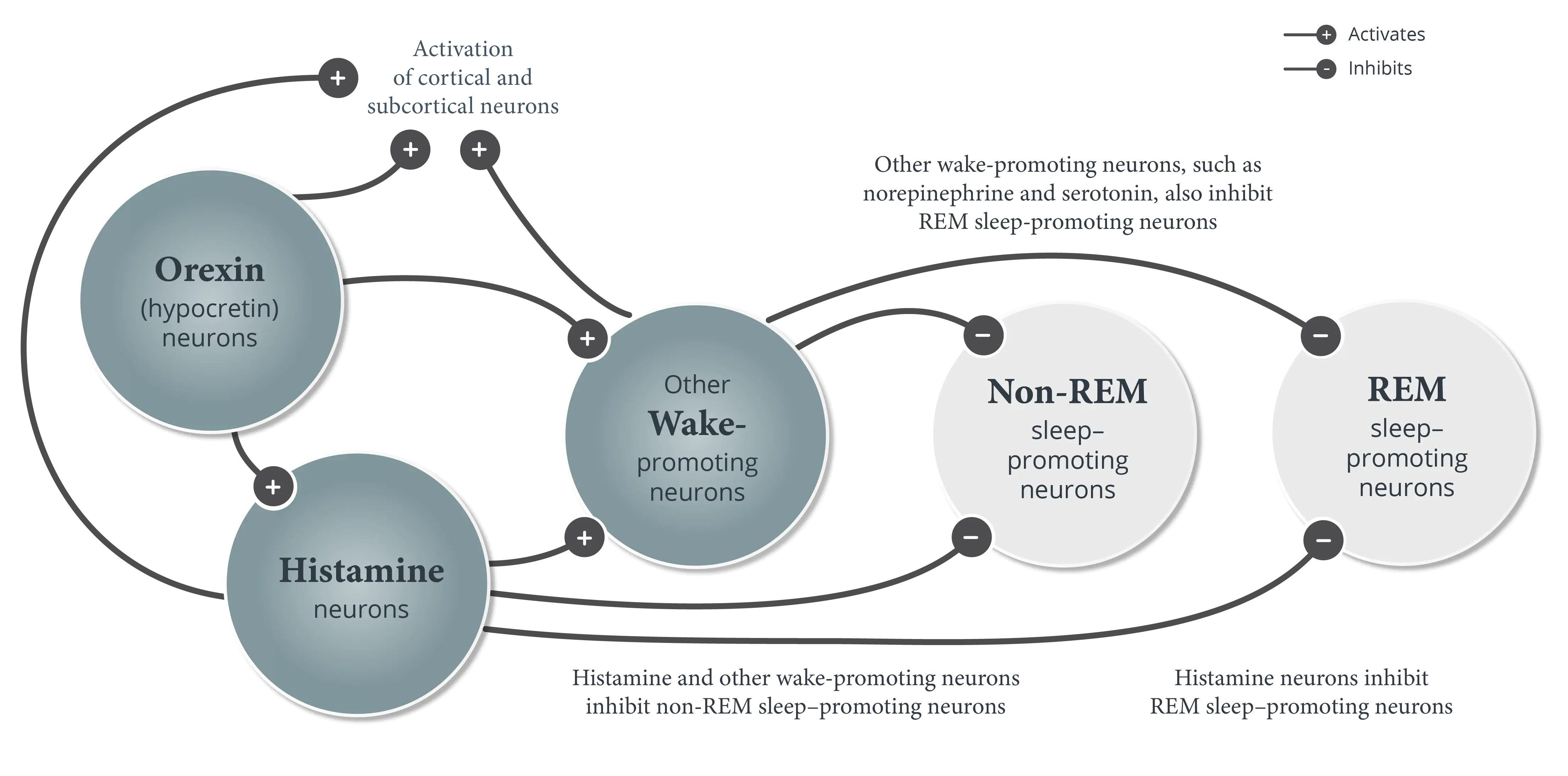
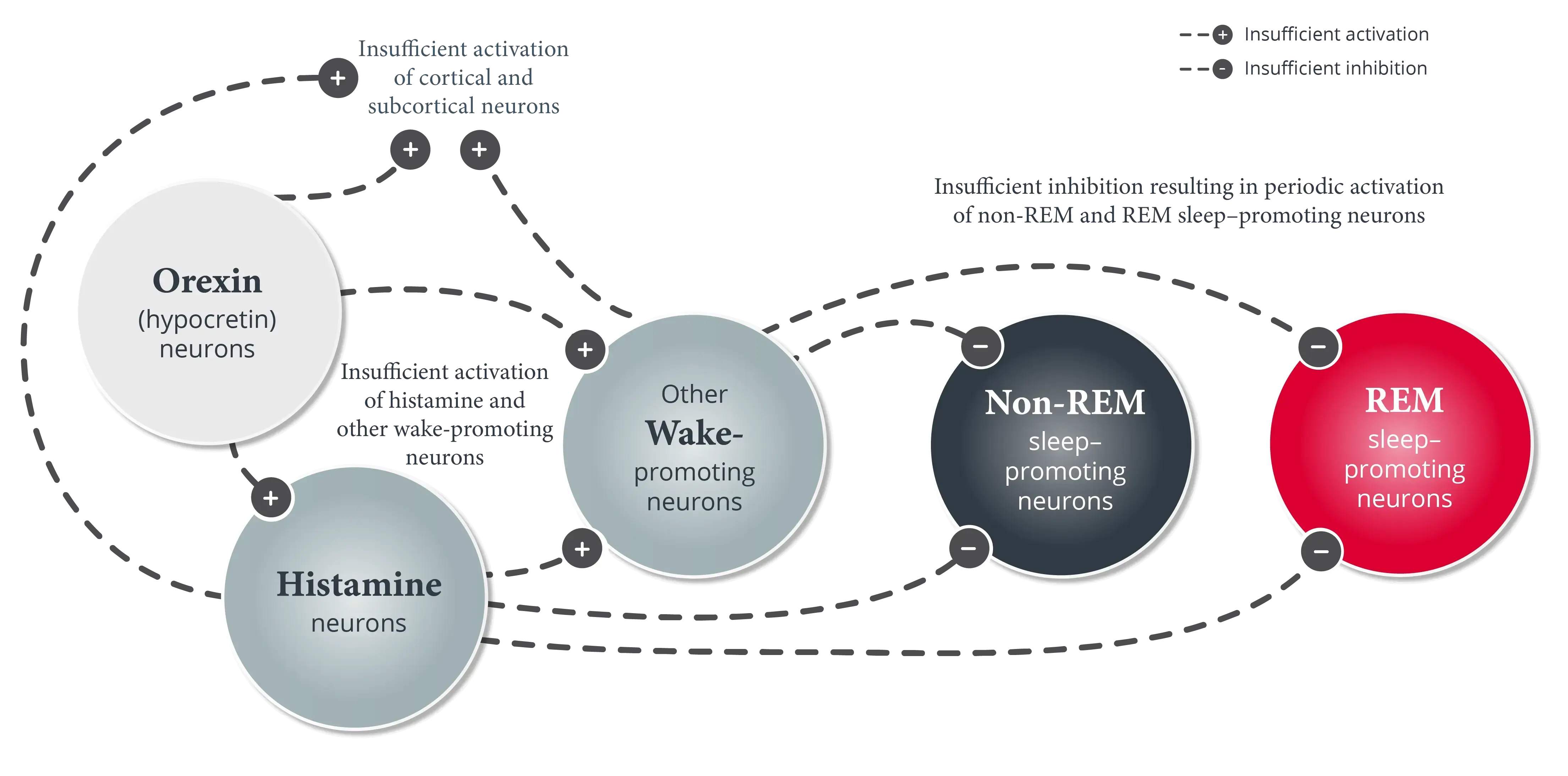
Narcolepsy is a chronic and lifelong neurologic disorder characterized by excessive daytime sleepiness (EDS) and abnormal manifestations of REM sleep.1,2 There are two types of narcolepsy—narcolepsy type 1 and narcolepsy type 2.1
Onset of narcolepsy typically begins after age 5, usually between the ages of 7 to 25. Symptom onset can be abrupt in children and may occur over the course of days or weeks. EDS is often the first symptom to appear.1


In addition to EDS, pediatric patients with narcolepsy type 1 experience cataplexy—a brief, bilaterally symmetrical, sudden loss of muscle tone with retained consciousness.1,2 When measured, levels of orexin (hypocretin) in the cerebrospinal fluid are generally undetectable or low.1
Cataplexy usually appears alongside EDS or within a year of onset, whereas other symptoms, such as hypnagogic hallucinations and sleep paralysis, generally appear later.1
Pediatric patients with narcolepsy type 2 do not have cataplexy, and their orexin (hypocretin) levels tend to be higher than in patients with narcolepsy type 1.1
Long-term management of narcolepsy in pediatric patients requires frequent assessment to monitor severity of symptoms and changes during treatment.5
A list of clinical resources is available, including subjective tests validated specifically in pediatric patients with narcolepsy.
Learn more about subtypes and pathophysiology of narcolepsy.
References
- American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd ed, text revision. American Academy of Sleep Medicine; 2023.
- Plazzi G, Clawges HM, Owens JA. Clinical characteristics and burden of illness in pediatric patients with narcolepsy. Pediatr Neurol. 2018;85:21-32.
- Maski K, Kotagal S. Clinical features and diagnosis of narcolepsy in children. Clinical Decision Support | UpToDate | Wolters Kluwer. Updated July 29, 2024. Accessed January 6, 2025. https://www.uptodate.com/contents/clinical-features-and-diagnosis-of-narcolepsy-in-children
- Chung I-H, Chin W-C, Huang Y-S, Wang C-H. Pediatric narcolepsy–a practical review. Children (Basel). 2022;9(7):974. doi:10.3390/children9070974
- Ouyang H, Gao X, Zhang J. Symptom measures in pediatric narcolepsy patients: a review. Ital J Pediatr. 2021;47(1):124. doi:10.1186/s13052-021-01068-7