More to Know: Cataplexy in Pediatric Patients
This content was developed using the International Classification of Sleep Disorders, third edition, text revision (ICSD-3-TR) and other materials.
More to Know: Cataplexy in Pediatric Patients
This content was developed using the International Classification of Sleep Disorders, third edition, text revision (ICSD-3-TR) and other materials.
Overview
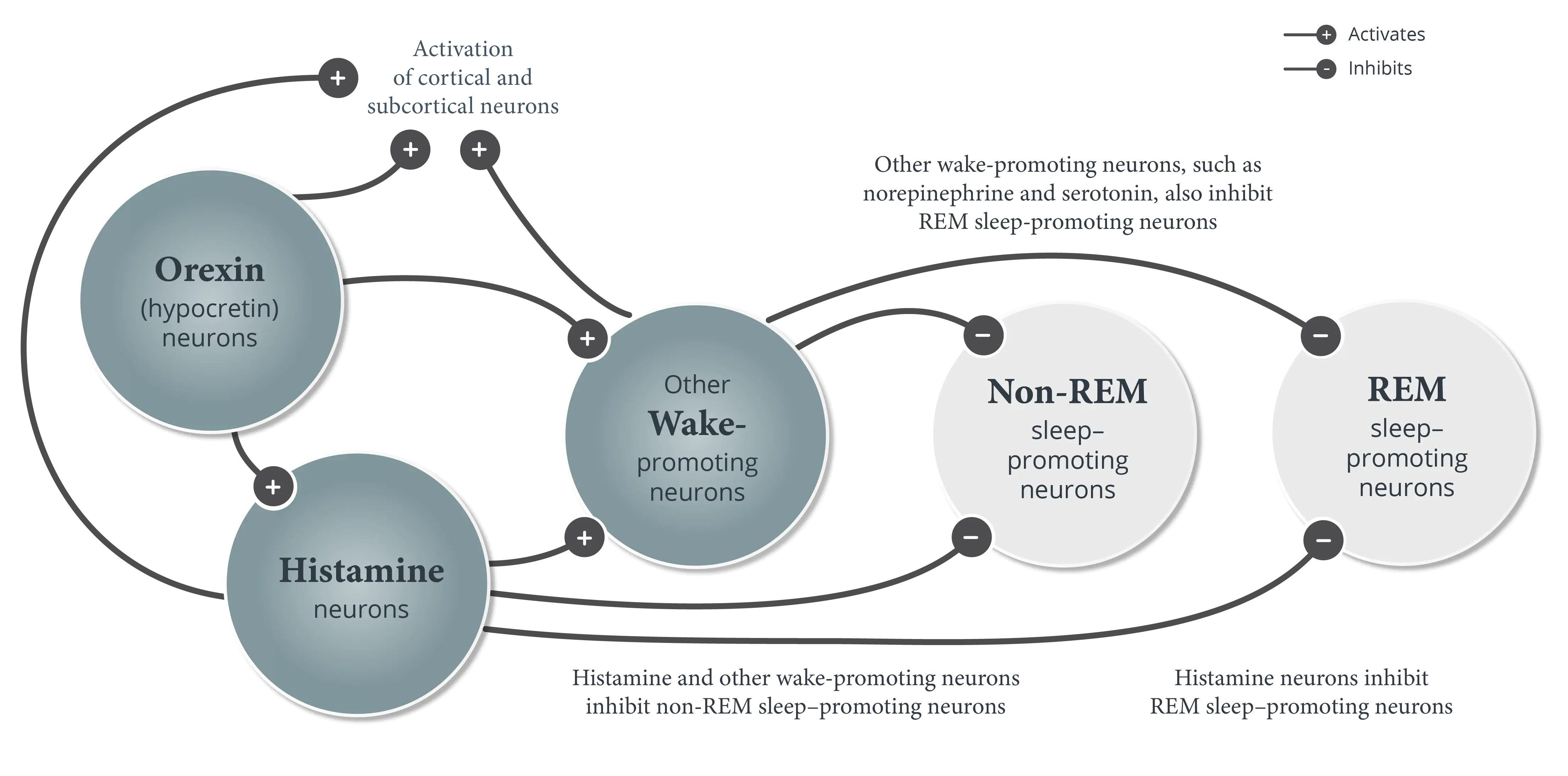
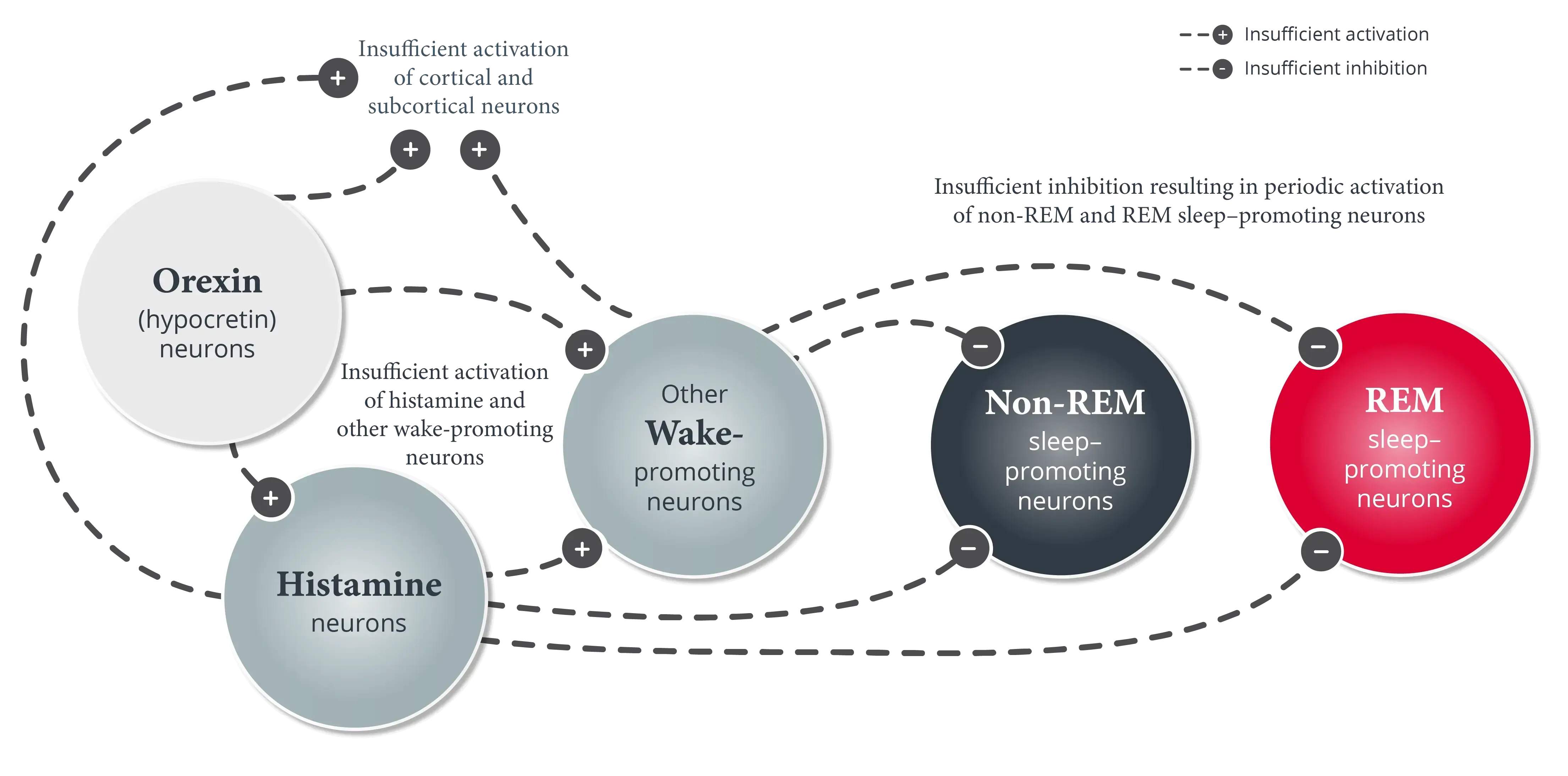
Cataplexy is present in approximately 70% to 80% of pediatric patients with narcolepsy and may manifest differently compared with adult patients.1-3
In addition to excessive daytime sleepiness (EDS), pediatric patients with narcolepsy type 1 experience cataplexy.1,4 Cataplexy is defined as more than one episode of generally brief (<2 minutes), usually bilaterally symmetrical, sudden loss of muscle tone with retained consciousness.1 Cataplexy onset may appear very close to the onset of EDS and can be severe.1,2
Cataplexy generally manifests as muscle weakness in the face, neck, or legs and is typically triggered by strong emotions, particularly those associated with laughter.1,2 Episodes tend to be short, lasting a few seconds up to 1 minute, followed by an abrupt return of muscle tone; consciousness is typically preserved. Some patients experience more than 20 cataplexy episodes per day.1
Cataplexy can manifest differently in pediatric patients compared with adult patients.1 For example, pediatric patients may experience “cataplectic facies,” a collective term that includes weakness involving the face, eyelids, and mouth with tongue protrusion; this form of cataplexy is not always clearly triggered by an emotion.1,2
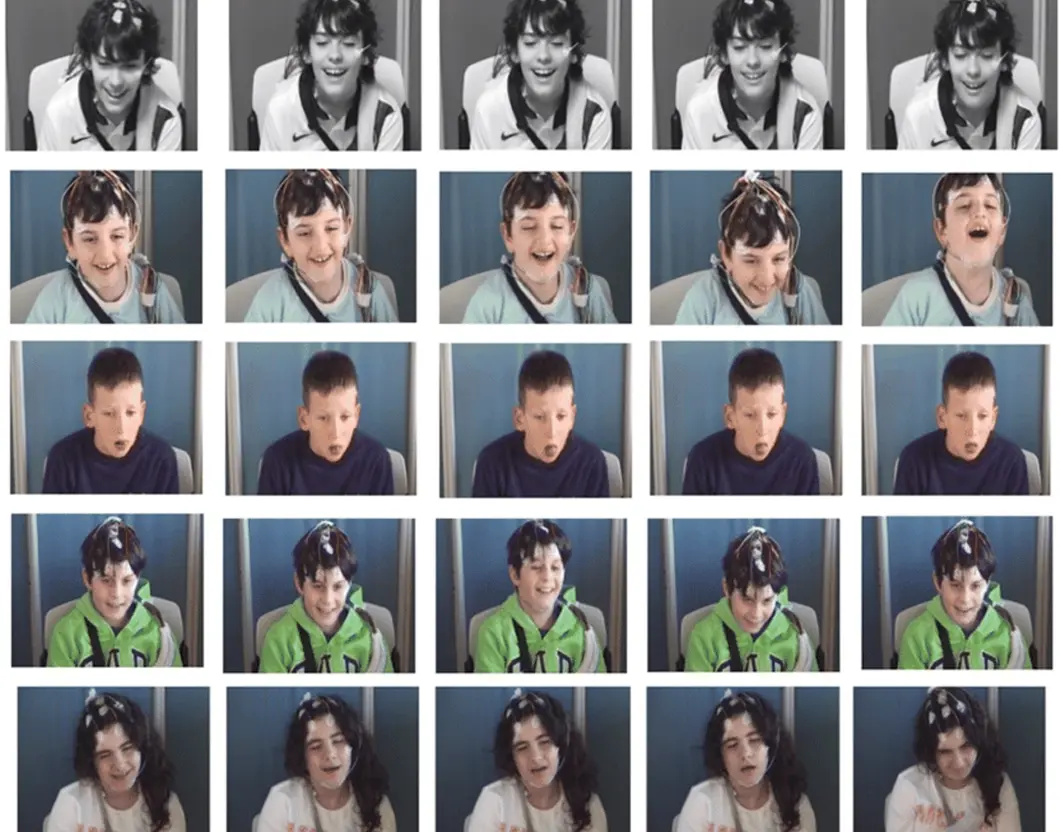
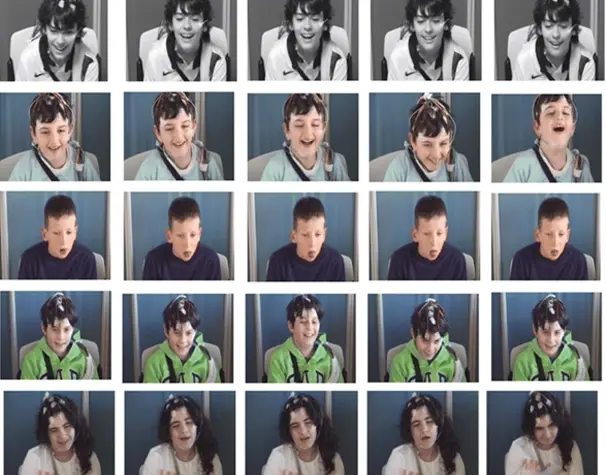
Images courtesy of Postiglione E et al. Sleep Med Rev. 2018;28:70-85.
Other cataplexy manifestations in pediatric patients with narcolepsy may include positive motor phenomena, such as1,2:
- Eyebrow raising2
- Movements of the mouth or surrounding area2
- Head or trunk swaying2
Pediatric patients may also experience complete cataplexy, which may cause falls or injuries.3
Episodes of cataplexy in pediatric patients can sometimes be confused with clumsiness, seizures, or neuromuscular disorders.4
References
- American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd ed, text revision. American Academy of Sleep Medicine; 2023.
- Maski K, Kotagal S. Clinical features and diagnosis of narcolepsy in children. Clinical Decision Support | UpToDate | Wolters Kluwer. Updated July 29, 2024. Accessed January 6, 2025. https://www.uptodate.com/contents/clinical-features-and-diagnosis-of-narcolepsy-in-children
- Chung I-H, Chin W-C, Huang Y-S, Wang C-H. Pediatric narcolepsy–a practical review. Children (Basel). 2022;9(7):974. doi:10.3390/children9070974
- Plazzi G, Clawges HM, Owens JA. Clinical characteristics and burden of illness in pediatric patients with narcolepsy. Pediatr Neurol. 2018;85:21-32.