Objective Findings in Adult Patients With Narcolepsy
This content was developed using the International Classification of Sleep Disorders, third edition, text revision (ICSD-3-TR) and the “American Academy of Sleep Medicine (AASM) recommended protocol for the Multiple Sleep Latency Test (MSLT),” published in Journal of Clinical Sleep Medicine (2021).
Objective Findings in Adult Patients With Narcolepsy
This content was developed using the International Classification of Sleep Disorders, third edition, text revision (ICSD-3-TR) and the “American Academy of Sleep Medicine (AASM) recommended protocol for the Multiple Sleep Latency Test (MSLT),” published in Journal of Clinical Sleep Medicine (2021).
Overview
Objective sleep testing with a Multiple Sleep Latency Test (MSLT) preceded by nighttime polysomnogram (PSG) is typically required for a narcolepsy diagnosis.1
The International Classification of Sleep Disorders, third edition, text revision (ICSD-3-TR) diagnostic criteria require results from objective sleep laboratory testing to support a narcolepsy diagnosis.1 An MSLT, which measures the patient’s physiologic tendency to fall asleep under standardized conditions, is the primary objective measure.1,2
A mean MSLT sleep latency of ≤8 minutes defines pathological sleepiness for the purposes of a narcolepsy diagnosis, but it is not diagnostic unless there is also objective evidence of REM sleep dissociation, the occurrence of sleep-onset REM periods (SOREMPs).1


Multiple SOREMPs during an MSLT are more specific to narcolepsy than short sleep latency. However, SOREMPs may also be observed with insufficient sleep, circadian rhythm sleep-wake disorders, sleep-related breathing disorders, using or withdrawing from certain substances/medications, or in individuals without narcolepsy. Therefore, a patient’s MSLT results should be considered alongside the patient’s medical history and clinical history, rather than being solely relied upon for diagnosis.1
MSLTs should be conducted based on standardized procedures that are defined in the American Academy of Sleep Medicine (AASM) recommended protocol.1,2 Patients should be encouraged to obtain adequate sleep during the preceding week and especially during the night prior to the MSLT.1 It is recommended that adequate sleep is documented by sleep log and actigraphy, whenever possible, for 1 to 2 weeks prior to conducting the MSLT.2
Adequate sleep on the night prior to the MSLT should be documented on overnight PSG. The average amount of sleep required for healthy adults is ≥7 hours; the nighttime PSG should allow for a minimum of 7 hours of time in bed and a minimum of 6 hours of sleep, with timing that corresponds to the patient’s major sleep period. This may require delaying the start of the MSLT to accommodate a later termination of the PSG.2
The occurrence of ≥1 SOREMP on the overnight PSG in the presence of cataplexy is diagnostic for narcolepsy type 1, and can replace one of the 2 SOREMPs on the MSLT required for a diagnosis of narcolepsy type 2.1
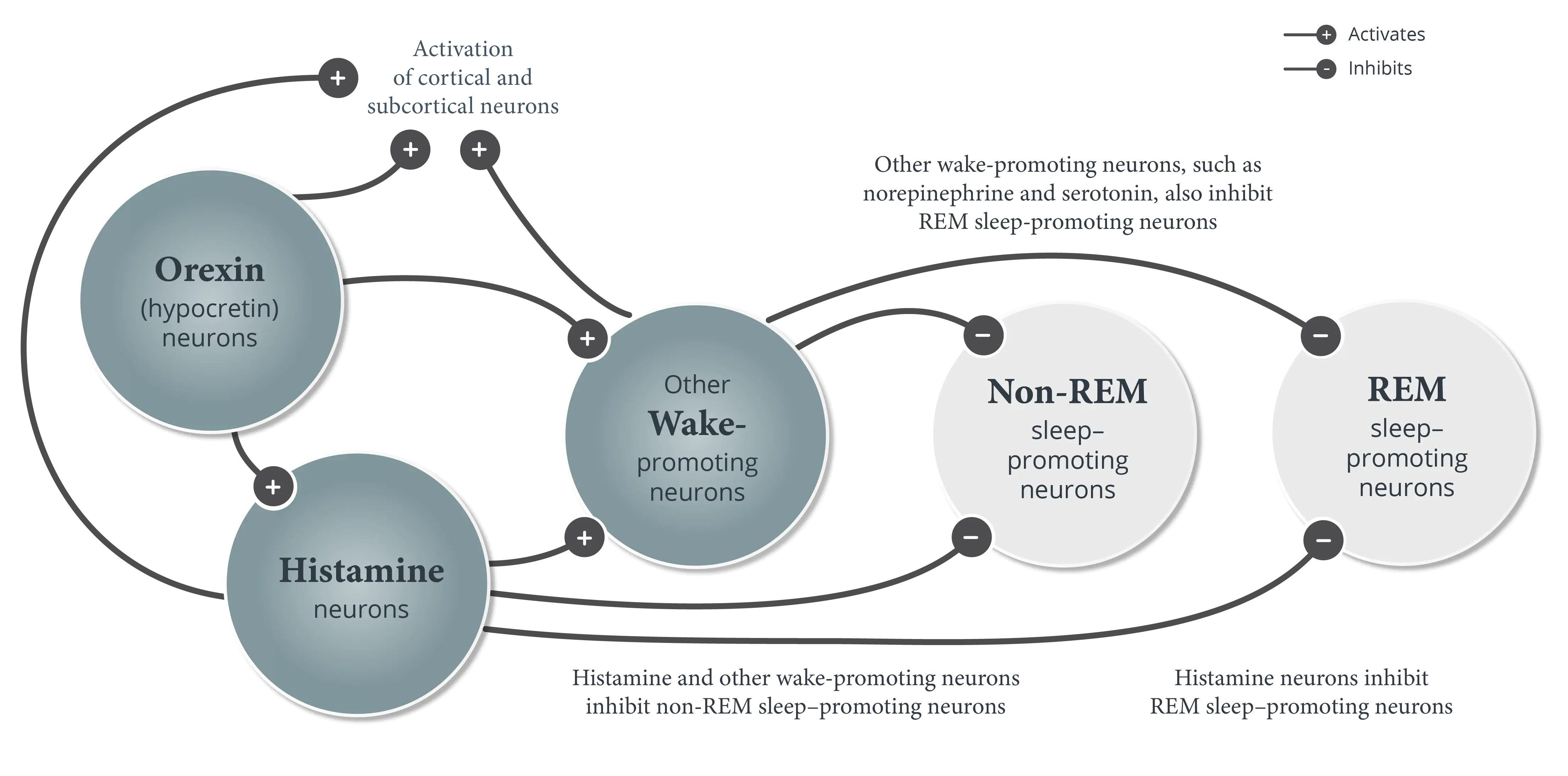
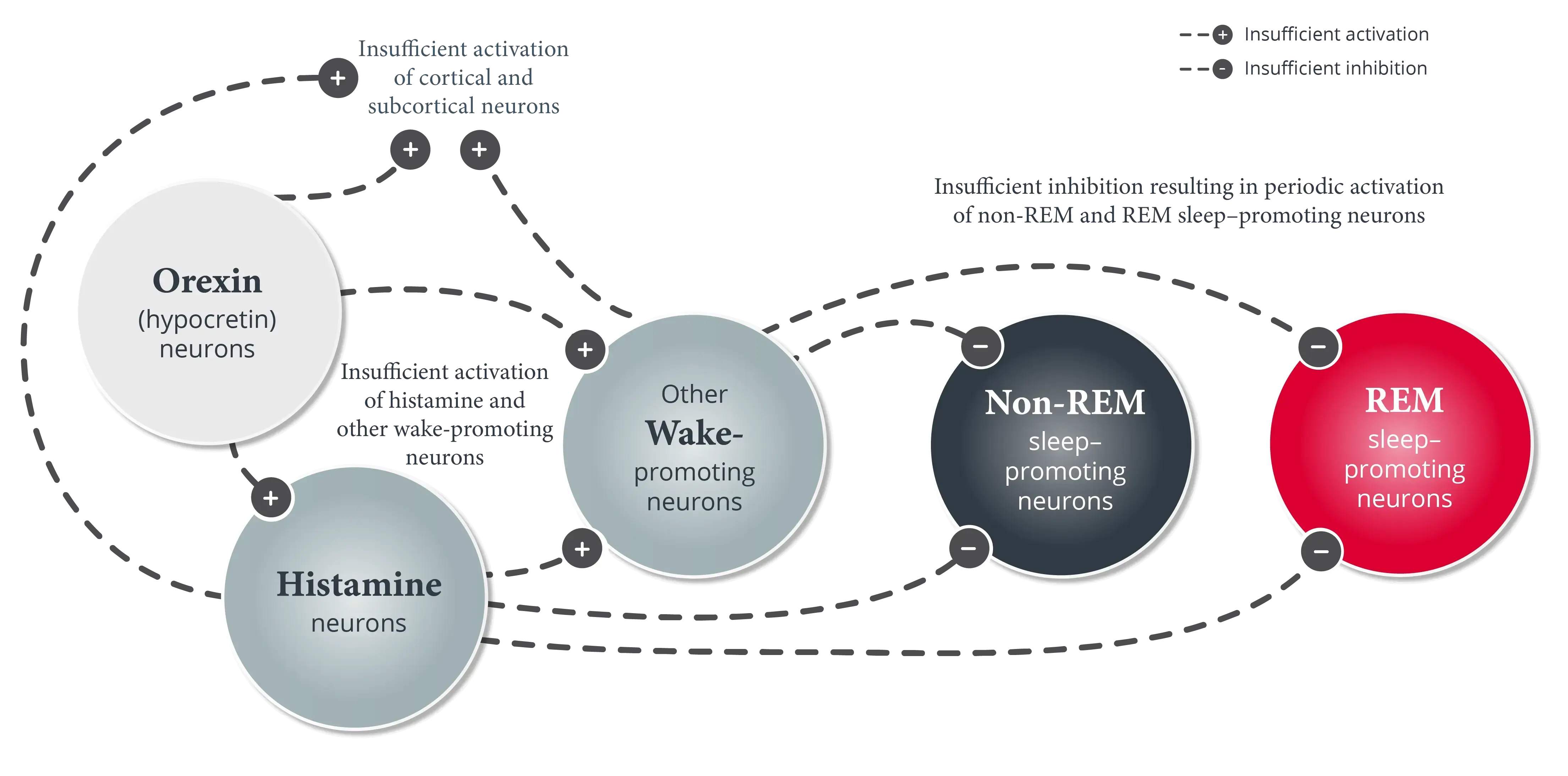
Narcolepsy is divided into narcolepsy type 1 and narcolepsy type 2 based on the concept that the presence of orexin (hypocretin) deficiency is a fundamental marker of narcolepsy type 1; however, CSF hypocretin-1 testing is not required for a narcolepsy diagnosis. If CSF hypocretin-1 is measured, the threshold for diagnosis of narcolepsy type 1 is ≤110 pg/mL or less than one-third of mean values obtained in normal subjects using the same standardized assay. Low CSF hypocretin-1 is diagnostic of narcolepsy in the presence of EDS that is not better explained by another sleep disorder, mental disorder, or medication/substance use or withdrawal.1
Objective sleep testing is essential for making a differential diagnosis of narcolepsy.1
References
- American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd ed, text revision. American Academy of Sleep Medicine; 2023.
- Krahn LE, Arand DL, Avidan AY, et al. Recommended protocols for the Multiple Sleep Latency Test and Maintenance of Wakefulness Test in adults: guidance from the American Academy of Sleep Medicine. J Clin Sleep Med. 2021;17(12):2489-2498.