Objective Findings in Pediatric Patients With Narcolepsy
This content was developed using “Recommended protocols for the Multiple Sleep Latency Test and Maintenance of Wakefulness Test in children: guidance from the American Academy of Sleep Medicine,” published in Journal of Clinical Sleep Medicine (2024), and other materials.
Objective Findings in Pediatric Patients With Narcolepsy
This content was developed using “Recommended protocols for the Multiple Sleep Latency Test and Maintenance of Wakefulness Test in children: guidance from the American Academy of Sleep Medicine,” published in Journal of Clinical Sleep Medicine (2024), and other materials.
Overview
Objective findings during sleep testing are required to confirm a diagnosis of narcolepsy in children and adolescents.1 The American Academy of Sleep Medicine (AASM) provides specific recommendations for diagnostic sleep testing in children and adolescents.2
Objective measurements are essential to making a narcolepsy diagnosis. Because patients with narcolepsy will potentially be on a treatment plan for the rest of their lives, confirming the correct diagnosis is important.1
The Multiple Sleep Latency Test (MSLT), preceded by an overnight polysomnogram (PSG), is part of a narcolepsy diagnosis; however, there are key considerations to keep in mind when conducting sleep laboratory testing in pediatric patients.1-3
The AASM protocol recommends ideally 2 weeks of adequate sleep documented by a sleep diary, or actigraphy if possible, before conducting the MSLT to determine if insufficient sleep may be causing the patient’s excessive daytime sleepiness (EDS). It is recommended that children and adolescents have a full night’s sleep (age-appropriate length of time) before the MSLT, confirmed by an attended overnight PSG performed during the patient’s normal sleep period. Long naps on the day of the PSG should be avoided.2
For pediatric patients, the PSG should allow for a minimum of 7 hours of sleep, with at least 8 hours of time in bed.2 The PSG may show increased stage N1 sleep, as well as disruptions to normal sleep patterns, including frequent awakenings.1
Interpreting MSLT and PSG results in pediatric patients is not always straightforward. False-positive or false-negative results can be caused by4:
- Lack of established normative values for the MSLT in prepubescent children
- Possibility of short mean sleep onset latency and sleep-onset REM periods (SOREMPs) in sleep-deprived adolescents who do not have narcolepsy
- Lack of understanding of or adherence to test instructions
For pediatric patients being evaluated for narcolepsy close to disease onset, more than one MSLT may be required before reaching a clear diagnosis.4
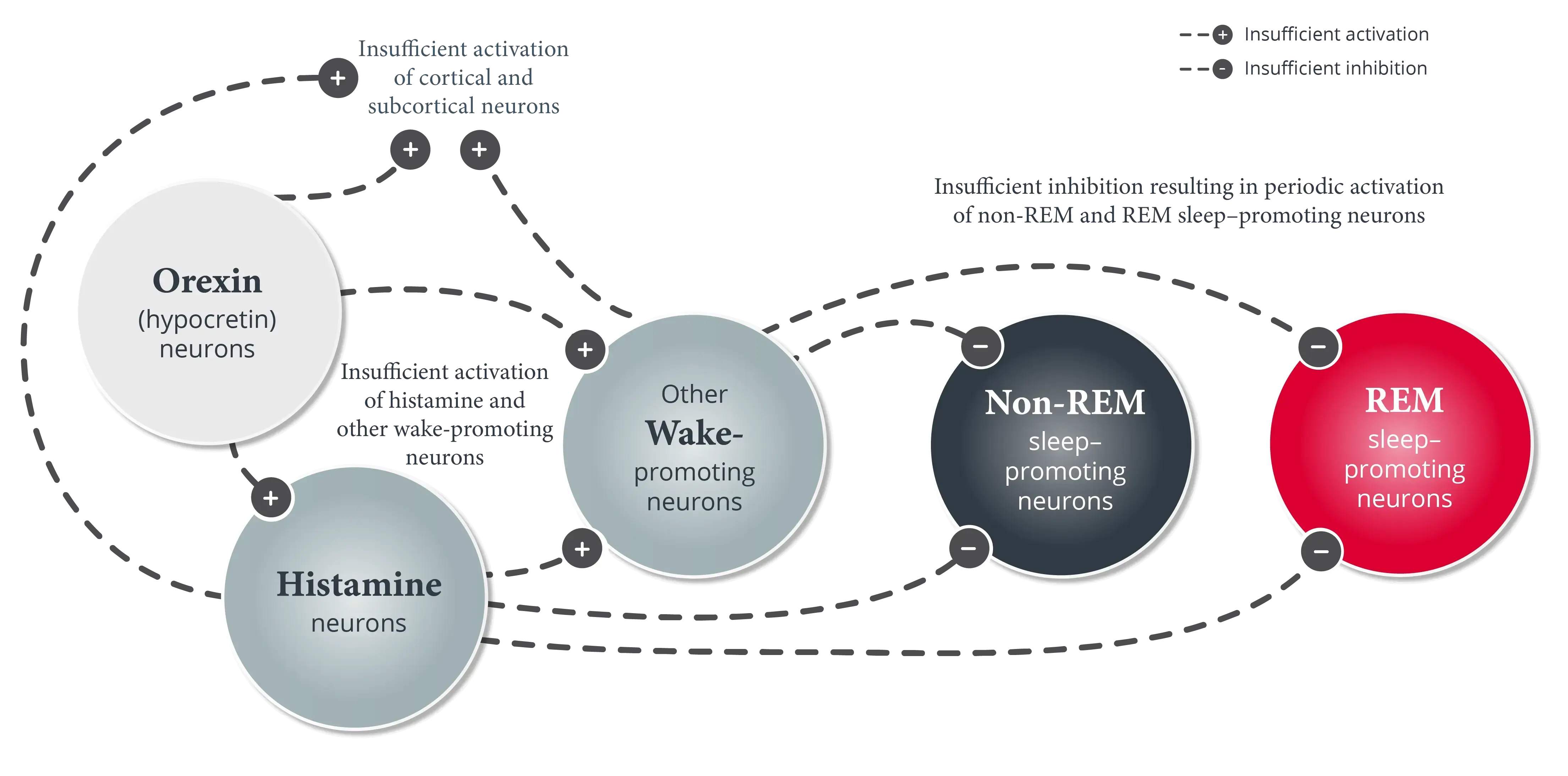
Additionally, low cerebrospinal fluid (CSF) hypocretin-1 levels are diagnostic for narcolepsy type 1 (narcolepsy with cataplexy) in patients with EDS. However, testing CSF hypocretin-1 levels is not required for diagnosis and is not sufficient for making a diagnosis of narcolepsy type 2 (narcolepsy without cataplexy).1
See additional information about making a differential diagnosis in pediatric patients.
References
- American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd ed, text revision. American Academy of Sleep Medicine; 2023.
- Maski KP, Amos LB, Carter JC, Koch EE, Kazmi U, Rosen CL. Recommended protocols for the Multiple Sleep Latency Test and Maintenance of Wakefulness Test in children: guidance from the American Academy of Sleep Medicine. J Clin Sleep Med. 2024;20(4):631-641.
- Krahn LE, Arand DL, Avidan AY, et al. Recommended protocols for the Multiple Sleep Latency Test and Maintenance of Wakefulness Test in adults: guidance from the American Academy of Sleep Medicine. J Clin Sleep Med. 2021;17(12):2489-2498.
- Plazzi G, Clawges HM, Owens JA. Clinical characteristics and burden of illness in pediatric patients with narcolepsy. Pediatr Neurol. 2018;85:21-32.